Alpha blocker
| Alpha blockers α-blockers | |
|---|---|
| Drug class | |
| Class identifiers | |
| Use | • Hypertension • Vasoconstriction • BPH • Raynaud's Disease • Pheochromocytoma • CHF • Erectile Dysfunction |
| Mechanism of action | • Receptor antagonist • Inverse agonist • Neutral antagonist |
| Biological target | α-adrenoceptors |
| Legal status | |
| In Wikidata | |

Alpha blockers, also known as α-blockers or α-adrenoreceptor antagonists, are a class of pharmacological agents that act as antagonists on α-adrenergic receptors (α-adrenoceptors).[2]
Historically, alpha-blockers were used as a tool for pharmacologic research to develop a greater understanding of the autonomic nervous system. Using alpha blockers, scientists began characterizing arterial blood pressure and central vasomotor control in the autonomic nervous system.[3] Today, they can be used as clinical treatments for a limited number of diseases.[2]
Alpha blockers can treat a small range of diseases such as hypertension, Raynaud's disease, benign prostatic hyperplasia (BPH) and erectile dysfunction.[2] Generally speaking, these treatments function by binding an α-blocker to α receptors in the arteries and smooth muscle. Ultimately, depending on the type of alpha receptor, this relaxes the smooth muscle or blood vessels, which increases fluid flow in these entities.[2]
Classification
[edit]
- α1-blockers act on α1-adrenoceptors
- α2-blockers act on α2-adrenoceptors
When the term "alpha blocker" is used without further qualification, it can refer to an α1 blocker, an α2 blocker, a nonselective blocker (both α1 and α2 activity), or an α blocker with some β activity.[2] However, the most common type of alpha blocker is usually an α1 blocker.
Non-selective α-adrenergic receptor antagonists include:
Selective α1-adrenergic receptor antagonists include:
Selective α2-adrenergic receptor antagonists include:
Finally, the agents carvedilol and labetalol are both α and β-blockers.
Below are some of the most common drugs used in the clinic.
| Drug Name | Common Brands | Structure | Mechanism of Action | Effects | Clinical Applications | Toxicity |
|---|---|---|---|---|---|---|
| Phenoxybenzamine | Dibenzyline |  | Nonselective covalent binding to α1 and α2 receptors. | Lowers blood pressure by decreasing peripheral resistance. Blocks alpha induced vasconstriction.[2] |
|
|
| Phentolamine | Regitine |  | Competitive blocking of α1 and α2 receptors. | Reversal of epinephrine induced effects. Lowers blood pressure by decreasing peripheral resistance.[2][10] |
| |
| Prazosin | Minipress | 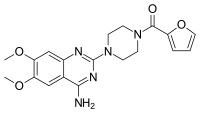 | Inverse agonist of α1 receptor.[10] | Lowers blood pressure.[2] | ||
| Doxazosin | Cardura Cardura XL | 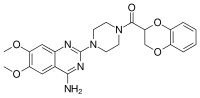 | Competitive blocking of α1 receptor.[10] | Lowers blood pressure.[2] |
| |
| Terazosin | Hytrin |  | Competitive blocking of α1 receptor.[10] | Lowers blood pressure.[2] | ||
| Tamsulosin | Flomax |  | A blocker that has slight selectivity for α1 receptors.[2] | Relaxation of prostatic smooth muscle.[2] |
| |
| Yohimbine | Yocon |  | Blocks α2 receptor, and increases norepinephrine release, thus increasing CNS activity.[2] | Raises blood pressure and heart rate.[2] |
| |
| Labetalol | Trandate |  | Blocks some α1 receptor activity, but binds more strongly to β receptors.[2] | Lowers blood pressure, increases heart rate slightly.[2] |
| |
| Carvedilol | Coreg Coreg CR |  | Blocks some α1 receptor activity, but binds more strongly to β receptors.[2] | Can interfere with noradrenergic mechanisms.[2] |
|
Medical uses
[edit]While there are limited clinical α-blocker uses, in which most α-blockers are used for hypertension or benign prostatic hyperplasia, α-blockers can be used to treat a few other diseases, such as Raynaud's disease, congestive heart failure (CHF), pheochromocytoma, and erectile dysfunction.[15][16][17]
Furthermore, α-blockers can occasionally be used to treat anxiety and panic disorders, such as posttraumatic stress disorder (PTSD) induced nightmares.[6] Studies have also had great medical interest in testing alpha blockers, specifically α2 blockers, to treat type II diabetes and psychiatric depression.[2]
Hypertension
[edit]Hypertension is due to an increase in vascular resistance and vasoconstriction. Using α1 selective antagonists, such as prazosin, has been efficacious in treating mild to moderate hypertension. This is because they can decrease vascular resistance and decrease pressure.[2][18] However, while these drugs are generally well tolerated, they have the potential to produce side effects such as orthostatic hypotension and dizziness.[2] However, unlike other treatments for hypertension such as ACE inhibitors, ARBs, calcium channel blockers, thiazide diuretics or beta blockers, alpha blockers have not demonstrated the same mortality and morbidity benefits, and are therefore not generally used as first or even second line agents.
Another treatment for hypertension is using drugs that have both α1 blocking activity, as well as nonselective β activity, such as Labetalol or carvedilol.[19] In low doses, labetalol and carvedilol can decrease the peripheral resistance and block the effects of isoprenaline to reduce hypertensive symptoms.[19]
Pheochromocytoma
[edit]
Pheochromocytoma is a disease in which a catecholamine secreting tumor develops.[2][20] Specifically, norepinephrine and epinephrine are secreted by these tumors, either continuously or intermittently.[21] The excess release of these catecholamines increases central nervous system stimulation, thus causing blood vessels to increase in vascular resistance, and ultimately giving rise to hypertension.[20] In addition, patients with these rare tumors are often subject to headaches, heart palpitations, and increased sweating.[2]
Phenoxybenzamine, a nonselective α1 and α2 blocker, has been used to treat pheochromocytoma.[21] This drug blocks the activity of epinephrine and norepinephrine by antagonizing the alpha receptors, thus decreasing vascular resistance, increasing vasodilation, and decreasing blood pressure overall.[21]
Congestive heart failure
[edit]Blockers that have both the ability to block both α and β receptors, such as carvedilol, bucindolol, and labetalol, have the ability to mitigate the symptoms in congestive heart failure.[22] By binding to both the α and β receptors, these drugs can decrease the cardiac output and stimulate the dilation of blood vessels to promote a reduction in blood pressure.[22]
Erectile dysfunction
[edit]Yohimbine, an α2 blocker derived from the bark of the Pausinystalia johimbe tree, has been tested to increase libido and treat erectile dysfunction. The proposed mechanism for yohimbine is blockade of the adrenergic receptors that are associated with neurotransmitters inhibition, including dopamine and nitric oxide, and thus aiding with penile erection and libido.[23] By doing so, they can alter the blood flow in the penis to aid in achieving an erection. However, some side effects can occur, such as palpitation, tremor, elevated blood pressure, and anxiety.[23] Yohimbe bark contains both α1 and α2 adrenergic receptors blocking alkaloids.
Phentolamine, a non-selective alpha blocker, has also been tested to treat erectile dysfunction. By reducing vasoconstriction in the penis, there appears to be increased blood flow that aids in penile erection. Side effects associated with phentolamine include headache, flushing, and nasal congestion.[23]

Phenoxybenzamine, a non-competitive α1 and α2 blocker was used by Dr. Giles Brindley in the first intracavernosal pharmacotherapy for erectile dysfunction.[24]
Benign prostatic hyperplasia
[edit]In benign prostatic hyperplasia (BPH), men experience urinary obstruction and are unable to urinate, thus leading to urinary retention.[2] α1 specific blockers have been used to relax the smooth muscle in the bladder and enlarged prostate.[25] Prazosin, doxazosin, and terazosin have been particularly useful for patients with BPH, especially in patients with hypertension.[2] In such patients, these drugs can treat both conditions at the same time.[2] In patients without hypertension, tamsulosin can be used, as it has the ability to relax the bladder and prostate smooth muscle without causing major changes in blood pressure.[25]
Raynaud's disease
[edit]
Both α1 blockers and α2 blockers have been examined to treat Raynaud's disease. Although α1 blockers, such as prazosin, have appeared to give slight improvement for the sclerotic symptoms of Raynaud's disease, there are many side effects that occur while taking this drug. Conversely, α2 blockers, such as yohimbine, appear to provide significant improvement of the sclerotic symptoms in Raynaud's Disease without excessive side effects.[26]
Post traumatic stress disorder
[edit]Patients with posttraumatic stress disorder (PTSD) have often continued to be symptomatic despite being treated with PTSD-specific drugs.[27] In addition, PTSD patients often have debilitating nightmares that continue, despite their treatments.[27] High doses of the α1 blocker, prazosin, have been efficacious in treating patients with PTSD induced nightmares due to its ability to block the effects of norepinephrine.[27]
Adverse effects of prazosin to treat PTSD nightmares include dizziness, first dose effect (a sudden loss of consciousness), weakness, nausea, and fatigue.[27]
Adverse effects
[edit]Although alpha blockers have the ability to reduce some disease pathology, there are some side effects that come with these alpha blockers.[28] However, because there are several structural compositions that make each alpha blocker different, the side effects are different for each drug. Side effects that arise when taking alpha blockers can include the first dose effect, cardiovascular side effects, genitourinary side effects, as well as other side effects.[28]
First dose effect
[edit]One of the most common side effects with alpha blockers is the first dose effect.[29] This is a phenomenon in which patients with hypertension take an alpha blocker for the first time, and suddenly experience an intense decrease in blood pressure. Ultimately, this gives rise to orthostatic hypotension, dizziness, and a sudden loss of consciousness due to the drastic drop in blood pressure.[29]
Alpha blockers that possess these side effects include prazosin, doxazosin, and terazosin.[30]
Cardiovascular side effects
[edit]There are some alpha blockers that can give rise to changes in the cardiovascular system, such as the induction of reflex tachycardia, orthostatic hypotension, or heart palpitations via alterations of the QT interval.[28][31] Alpha blockers that may have these side effects include yohimbine, phenoxybenzamine, and phentolamine.[2]
Genitourinary side effects
[edit]When alpha blockers are used to treat BPH, it causes vasodilation of blood vessels on the bladder and the prostate, thus increasing urination in general.[32] However, these alpha blockers can produce the exact opposite side effect, in which edema, or abnormal fluid retention, occurs.[33]
In addition, due to the relaxation of the prostate smooth muscle, another side effect that arises in men being treated for BPH is impotence, as well as the inability to ejaculate.[32][34] However, if any ejaculation activity does occur, oftentimes, it results in a phenomenon called retrograde ejaculation, in which semen flows into the urinary bladder instead of exiting through the urethra.[34]
Drugs that may produce such side effects include prazosin, terazosin, tamsulosin, and doxazosin.[34]
Other side effects
[edit]Finally, there are other general side effects that can be caused by most alpha blockers (however, more frequently in alpha-1 blockers). Such side effects include dizziness, drowsiness, weakness, fatigue, psychiatric depression, and dry mouth.[28][34]
Priapism, an unwanted, painful long term erection not brought on by sexual arousal and lasting several hours has been associated with alpha blocker use. While this is extremely rare, particularly with tamsulosin, it can cause permanent impotence if not treated in a hospital setting. Male patients should be made aware of this as it can result from a single dose or develop over time.
Contraindications
[edit]There is only one compelling indication for alpha blockers, which is for benign prostatic hyperplasia.[33] Patients who need alpha blockers for BPH, but have a history of hypotension or postural heart failure, should use these drugs with caution, as it may result in an even greater decrease in blood pressure or make heart failure even worse.[35][36] The most compelling contraindication is urinary incontinence and overall fluid retention.[35][36] To combat such fluid retention, patients can take a diuretic in combination with the alpha-blocker.[36]
In the absence of compelling indications or contraindications, patients should take alpha blockers as a step 4 therapy to reduce blood pressure, but only if the use of ACE inhibitors, angiotensin-II receptor blockers, calcium channel blockers, or thazide diuretics (in full dose or in combinations) have not been efficacious.[33][35][36]
Drug interactions
[edit]As with any drug, there are drug interactions that can occur with alpha blockers. For instance, alpha blockers that are used for the reduction of blood pressure, such as phenoxybenzamine or phentolamine can have synergy with other drugs that affect smooth muscle, blood vessels, or drugs used for erectile dysfunction (i.e. sildenafil, tamsulosin, etc.). This stimulates exaggerated hypotension.[2]
Alternative alpha blockers, such as prazosin, tamsulosin, doxazosin, or terazosin can have adverse interactions with beta blockers, erectile dysfunction drugs, anxiolytics, and antihistamines.[2] Again, these interactions can cause dangerous hypotension. Furthermore, in rare cases, drug interactions can cause irregular, rapid heartbeats or an increase blood pressure.[2]
Yohimbine can interact with stimulants, hypertension drugs, naloxone, and clonidine. Interactions with such drugs can cause either an unintended increase in blood pressure or potentiate an increase in blood pressure.[2]
Finally, in drugs with both alpha and beta blocking properties, such as carvedilol and labetalol, interactions with other alpha or beta blockers can exaggerate a decrease in blood pressure.[2] Conversely, there are also drug interactions with carvedilol or labetalol in which blood pressure is increased unintentionally (such as with cough and cold medications).[2] Finally, there may also be some alpha/beta blocker drug interactions that can worsen previous heart failure.[2]
Mechanism of action
[edit]Alpha blockers work by blocking the effect of nerves in the sympathetic nervous system. This is done by binding to the alpha receptors in smooth muscle or blood vessels.[37] α-blockers can bind both reversibly and irreversibly.[2]
There are several α receptors throughout the body where these drugs can bind. Specifically, α1 receptors can be found in most vascular smooth muscle, the pupillary dilator muscle, the heart, the prostate, and pilomotor smooth muscle.[2] On the other hand, α2 receptors can be found in platelets, cholinergic nerve terminals, some vascular smooth muscle, postsynaptic CNS neurons, and fat cells.[2]
The structure of α receptors is a classic G protein–coupled receptors (GPCRs) consisting of 7 transmembrane domains, which form three intracellular loops and three extracellular loops.[2] These receptors couple to heterotrimeric G proteins composed of α, β, and γ subunits.[2] Although both of the α receptors are GPCRs, there are large differences in their mechanism of action. Specifically, α1 receptors are characterized as Gq GPCRs, signaling through Phospholipase C to increase IP3 and DAG, thus increasing the release of calcium. Meanwhile, α2 receptors are labeled as Gi GPCRs, which signal through adenylyl cyclase to decrease cAMP.[38]
Because the α1 and α2 receptors have different mechanisms of action, their antagonists also have different effects.[39] α1 blockers can inhibit the release of IP3 and DAG to decrease calcium release, thus, decreasing overall signaling. On the other hand, α2 blockers prevent the reduction of cAMP, thus leading to an increase in overall signaling.
 |  |
|---|
See also
[edit]References
[edit]- ^ Katzung B (1987). Basic and Clinical Pharmacology. Appleton & Lange. ISBN 9780838505533.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc Katzung B, Masters S (2013). Basic and Clinical Pharmacology. Lange. ISBN 978-0-07-176402-5.
- ^ Bousquet P, Schwartz J (May 1983). "Alpha-adrenergic drugs. Pharmacological tools for the study of the central vasomotor control". Biochemical Pharmacology. 32 (9): 1459–1465. doi:10.1016/0006-2952(83)90466-5. PMID 6134533.
- ^ McKeage K, Plosker GL (2002-03-01). "Alfuzosin: a review of the therapeutic use of the prolonged-release formulation given once daily in the management of benign prostatic hyperplasia". Drugs. 62 (4): 633–653. doi:10.2165/00003495-200262040-00009. PMID 11893233. S2CID 250307179.
- ^ a b Nash DT (November 1990). "Alpha-adrenergic blockers: mechanism of action, blood pressure control, and effects of lipoprotein metabolism". Clinical Cardiology. 13 (11): 764–772. doi:10.1002/clc.4960131104. PMID 1980236. S2CID 24619863.
- ^ a b c Green B (July 2014). "Prazosin in the treatment of PTSD". Journal of Psychiatric Practice. 20 (4): 253–259. doi:10.1097/01.pra.0000452561.98286.1e. PMID 25036580. S2CID 40069887.
- ^ "Tamsulosin Monograph for Professionals". Drugs.com. Archived from the original on 2021-01-20. Retrieved 29 January 2021.
- ^ a b Lepor H, Henry D, Laddu AR (1991-01-01). "The efficacy and safety of terazosin for the treatment of symptomatic BPH". The Prostate. 18 (4): 345–355. doi:10.1002/pros.2990180408. PMID 1711689. S2CID 37160206.
- ^ Michel MC (2010). "The Pharmacological Profile of the α1A-Adrenoceptor Antagonist Silodosin". European Urology Supplements. 9 (4): 486–490. doi:10.1016/j.eursup.2010.03.006.
- ^ a b c d e f g h i j k l Mycek MJ, Harvey RA, Champe PC (1997). Pharmacology (2nd ed.). Philadelphia: Lippincott-Raven. ISBN 978-0397515677. OCLC 34905985.
- ^ Narayan P, Tunuguntla HS (2005). "Long-term efficacy and safety of tamsulosin for benign prostatic hyperplasia". Reviews in Urology. 7 (Suppl 4): S42 – S48. PMC 1477608. PMID 16986054.
- ^ Charney DS, Woods SW, Goodman WK, Heninger GR (August 1987). "Neurobiological mechanisms of panic anxiety: biochemical and behavioral correlates of yohimbine-induced panic attacks". The American Journal of Psychiatry. 144 (8): 1030–1036. doi:10.1176/ajp.144.8.1030. PMID 3037926.
- ^ Richards DA (August 1976). "Pharmacological effects of labetalol in man". British Journal of Clinical Pharmacology. 3 (4 Suppl 3): 721–723. PMID 10949.
- ^ Cohn JN, Fowler MB, Bristow MR, Colucci WS, Gilbert EM, Kinhal V, et al. (September 1997). "Safety and efficacy of carvedilol in severe heart failure. The U.S. Carvedilol Heart Failure Study Group". Journal of Cardiac Failure. 3 (3): 173–179. doi:10.1016/s1071-9164(97)90013-0. PMID 9330125.
- ^ Roehrborn CG, Schwinn DA (March 2004). "Alpha1-adrenergic receptors and their inhibitors in lower urinary tract symptoms and benign prostatic hyperplasia". The Journal of Urology. 171 (3): 1029–1035. doi:10.1097/01.ju.0000097026.43866.cc. PMID 14767264.
- ^ Messerli FH (November 2001). "Doxazosin and congestive heart failure". Journal of the American College of Cardiology. 38 (5): 1295–1296. doi:10.1016/s0735-1097(01)01534-0. PMID 11691497.
- ^ Ernst E, Pittler MH (February 1998). "Yohimbine for erectile dysfunction: a systematic review and meta-analysis of randomized clinical trials". The Journal of Urology. 159 (2): 433–436. doi:10.1016/s0022-5347(01)63942-9. PMID 9649257.
- ^ Laurent S (October 2017). "Antihypertensive drugs". Pharmacological Research. 124: 116–125. doi:10.1016/j.phrs.2017.07.026. PMID 28780421. S2CID 251991.
- ^ a b Brogden RN, Heel RC, Speight TM, Avery GS (April 1978). "Labetalol: a review of its pharmacology and therapeutic use in hypertension". Drugs. 15 (4): 251–270. doi:10.2165/00003495-197815040-00002. PMID 25757. S2CID 42161040.
- ^ a b Bravo EL (September 2002). "Pheochromocytoma: an approach to antihypertensive management". Annals of the New York Academy of Sciences. 970 (1): 1–10. Bibcode:2002NYASA.970....1B. doi:10.1111/j.1749-6632.2002.tb04408.x. PMID 12381537. S2CID 222084372.
- ^ a b c Das S, Kumar P, Kiran U, Airan B (January 2017). "Alpha blockers: A relook at phenoxybenzamine". Journal of the Practice of Cardiovascular Sciences. 3 (1): 11. doi:10.4103/jpcs.jpcs_42_16.
- ^ a b Bristow MR (February 2000). "beta-adrenergic receptor blockade in chronic heart failure". Circulation. 101 (5): 558–569. doi:10.1161/01.CIR.101.5.558. PMID 10662755.
- ^ a b c Lue TF (June 2000). "Erectile dysfunction". The New England Journal of Medicine. 342 (24): 1802–1813. doi:10.1056/nejm200006153422407. PMID 10853004.
- ^ Carson CC, ed. (2007). "A Description of the Pioneering Work That Led to the First Approved Agents for ED: Giles Brindley, the Needle, and the Penis (Phenoxybenzamine)". Key Clinical Trials in Erectile Dysfunction. London: Springer. pp. 4–7. doi:10.1007/978-1-84628-428-1_2. ISBN 978-1-84628-428-1.
- ^ a b Chapple CR (January 1996). "Selective alpha 1-adrenoceptor antagonists in benign prostatic hyperplasia: rationale and clinical experience". European Urology. 29 (2): 129–144. PMID 8647139.
- ^ Bakst R, Merola JF, Franks AG, Sanchez M (October 2008). "Raynaud's phenomenon: pathogenesis and management". Journal of the American Academy of Dermatology. 59 (4): 633–653. doi:10.1016/j.jaad.2008.06.004. PMID 18656283.
- ^ a b c d Koola MM, Varghese SP, Fawcett JA (February 2014). "High-dose prazosin for the treatment of post-traumatic stress disorder". Therapeutic Advances in Psychopharmacology. 4 (1): 43–47. doi:10.1177/2045125313500982. PMC 3896131. PMID 24490030.
- ^ a b c d Manning L, Rayfield S. Pharmacology Made Easy. Bossier City, LA: ICAN. p. 38.
- ^ a b Hodsman GP, Isles CG, Murray GD, Usherwood TP, Webb DJ, Robertson JI (March 1983). "Factors related to first dose hypotensive effect of captopril: prediction and treatment". British Medical Journal. 286 (6368): 832–834. doi:10.1136/bmj.286.6368.832. PMC 1547159. PMID 6403103.
- ^ Elliott HL (2007). "Alpha Adrenoreceptor Antagonists". Comprehensive Hypertension. pp. 1019–1025. doi:10.1016/b978-0-323-03961-1.50085-4. ISBN 9780323039611.
- ^ Lepor H, Lepor NE, Hill LA, Trohman RG (Spring 2008). "The QT Interval and Selection of Alpha-Blockers for Benign Prostatic Hyperplasia". Reviews in Urology. 10 (2): 85–91. PMC 2483321. PMID 18660858.
- ^ a b Lepor H (Fall 2007). "Alpha blockers for the treatment of benign prostatic hyperplasia". Reviews in Urology. 9 (4): 181–190. PMC 2213889. PMID 18231614.
- ^ a b c "Alpha-blockers: their properties and use in hypertension". Prescriber. 22 (13–14): 38–39. July 2011. doi:10.1002/psb.779.
- ^ a b c d Debruyne FM (November 2000). "Alpha blockers: are all created equal?". Urology. 56 (5 Suppl 1): 20–22. doi:10.1016/s0090-4295(00)00744-5. PMID 11074198.
- ^ a b c "Alpha-Adrenoceptor Antagonists (Alpha-Blockers)" (PDF). British Hypertension Society. Archived from the original (PDF) on 2017-08-29.
- ^ a b c d "CV Pharmacology | Alpha-Adrenoceptor Antagonists (Alpha-Blockers)". cvpharmacology.com. Retrieved 2017-11-15.
- ^ Knott L (2015-06-27). "Alpha-blockers". Patient.
- ^ Pierce KL, Premont RT, Lefkowitz RJ (September 2002). "Seven-transmembrane receptors". Nature Reviews. Molecular Cell Biology. 3 (9): 639–650. doi:10.1038/nrm908. PMID 12209124. S2CID 23659116.
- ^ Bylund DB (February 1992). "Subtypes of alpha 1- and alpha 2-adrenergic receptors". FASEB Journal. 6 (3): 832–839. doi:10.1096/fasebj.6.3.1346768. PMID 1346768. S2CID 83827013.


 French
French Deutsch
Deutsch